1up Electronic Prior Authorization
Streamline prior authorization with a centralized hub for prior authorization requests

The current challenges
Your utilization management team needs an automated and standardized approach to handle prior authorizations with in-network providers. Automating this process can lead to operational efficiencies, reduced provider burden, and improved patient care.
However, prior authorization today relies on disparate, manual intake channels, which puts a heavy burden on providers and often lacks the necessary supporting clinical documentation. This results in a greater administrative burden on your UM team, clinician burnout, and delayed or abandoned treatment for patients.
Automate prior authorization for in-network providers
Designed to meet CMS Interoperability and Prior Authorization Final Rule (CMS-0057-F) requirements and leveraging industry standards, 1up’s Prior Authorization API automates the prior authorization process using a standard FHIR®-based API to connect in-network providers with your prior authorization rules and existing utilization management systems.
Our Prior Authorization solution enables provider partners to confirm whether prior authorization is necessary for a given service or procedure, discover specific prior authorization documentation requirements, and submit a prior authorization request with the required documentation to your utilization management team for review and receive a response.
With the 1up Prior Authorization API, you can:
Meet Regulatory Requirements
Adhere to CMS-0057-F compliance requirements for Prior Authorization

Streamline Processes
Shift from point-to-point connectivity with individual providers to centralized connectivity via 1upHealth
Realize Cost Savings
Eliminate manual processes and operational inefficiencies by limiting the number of denials or appeals and minimizing requests for additional documentation
Reduce Provider Burden
Enable providers to submit prior authorization requests faster and easier and receive more timely decisions
Improve Member Outcomes
Improve the quality of care for members by permitting faster scheduling of necessary services or filing appeals, depending on the decision
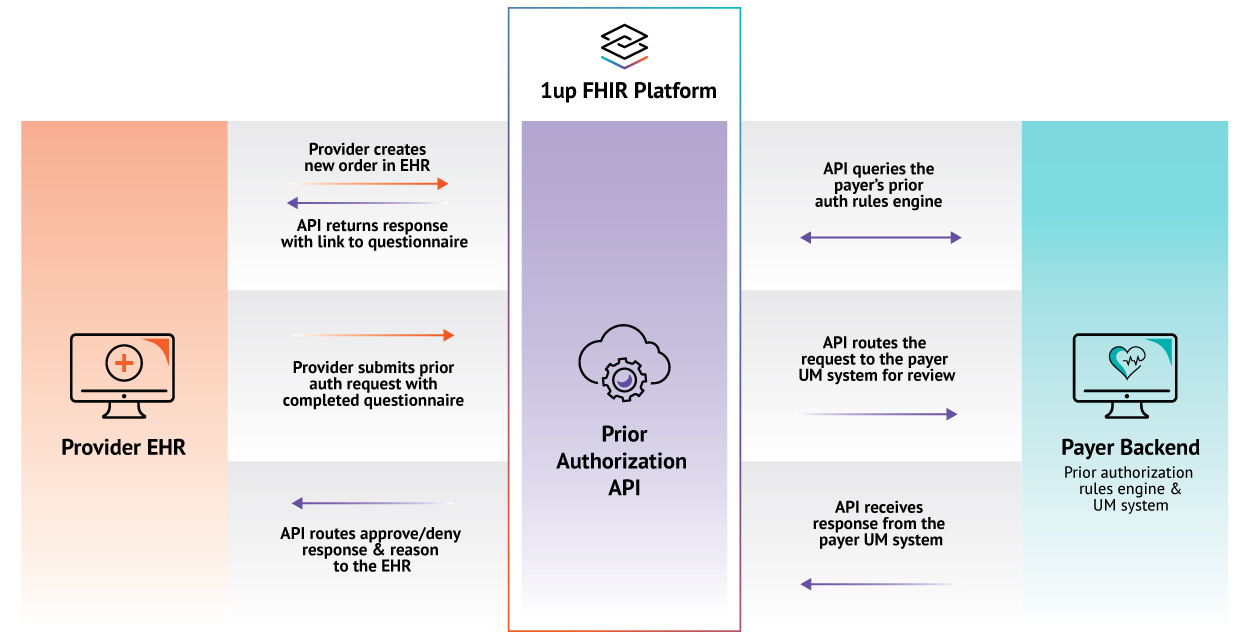
How 1up Prior Authorization Works
- A provider creates a new order for a service in the EHR, triggering a request to the 1up Prior Authorization API.
- The 1up API queries your prior authorization rules engine to determine if prior authorization is necessary and returns a response back to the EHR.
- If prior authorization is required, the response includes a link to a questionnaire that will automatically fill in the required clinical information from the patient record in the EHR.
- The provider verifies and augments the information in the questionnaire as necessary.
- They then submit the prior authorization request and the completed questionnaire via the 1up Prior Authorization API.
- The 1up API routes the request to your utilization management system for review and returns a decision (approval or denial), including the denial reason, to the provider’s EHR system.
Why 1up Prior Authorization
Centralized
Streamlines connectivity between payers and providers, creating a centralized hub for prior authorization requests
Standardized
Adheres to FHIR R4 and US Core standards for exchanging clinical data
Integrated
Allows for easy integration with your rules engine and existing utilization management systems