1up Payer-to-Payer Data Exchange API
Easily and securely exchange member data with other payers in a standardized format.

The current challenges of acquiring historical data
As you acquire new members, you need to know as much as possible about their clinical, claims, encounter, and prior authorization history. Historical data can inform care management, ensure continuity of care, create more targeted member experiences, and support operational priorities like risk adjustment and quality measures.
But, acquiring historical data from other payers is challenging, fraught with inefficient, manual processes and inconsistent data formats—leading to high administrative costs for your team. Similarly, it can be just as arduous to share your member data with other payers with whom you share concurrent or prior members.
1up Health makes it easy to exchange data with other payers
Designed to meet CMS Interoperability and Prior Authorization Final Rule (CMS-0057-F) requirements and leveraging industry standards, the 1up Payer-to-Payer Data Exchange API lets you easily and securely exchange member data with other payers in a standardized format—eliminating manual processes and administrative costs.
Our FHIR®-based API allows you to share and receive health data with other payers for new and previous members who have opted into data sharing, excluding cost-sharing and remittance dollar amounts. Incorporating data from other payers gives you a complete view of your member base and supports more informed and efficient decision-making.
With the 1up Payer-to-Payer Data Exchange API, you can:
Meet Regulatory Requirements
Adhere to CMS-0057-F compliance requirements for Payer-to-Payer Data Exchange

Streamline Processes
Eliminate manual processes and reduce administrative burden related to exchanging data with other payers
Provide Better Member Care
Make more informed decisions about member care management, ensure continuity of care, and identify care gaps for your members

Improve Risk Adjustment
More accurately assess risk levels of new and active members with access to historical clinical and claims data

Enhance Quality Measurement & Reporting
Improve performance against key quality measures via improved care coordination and targeted interventions based on historical member data
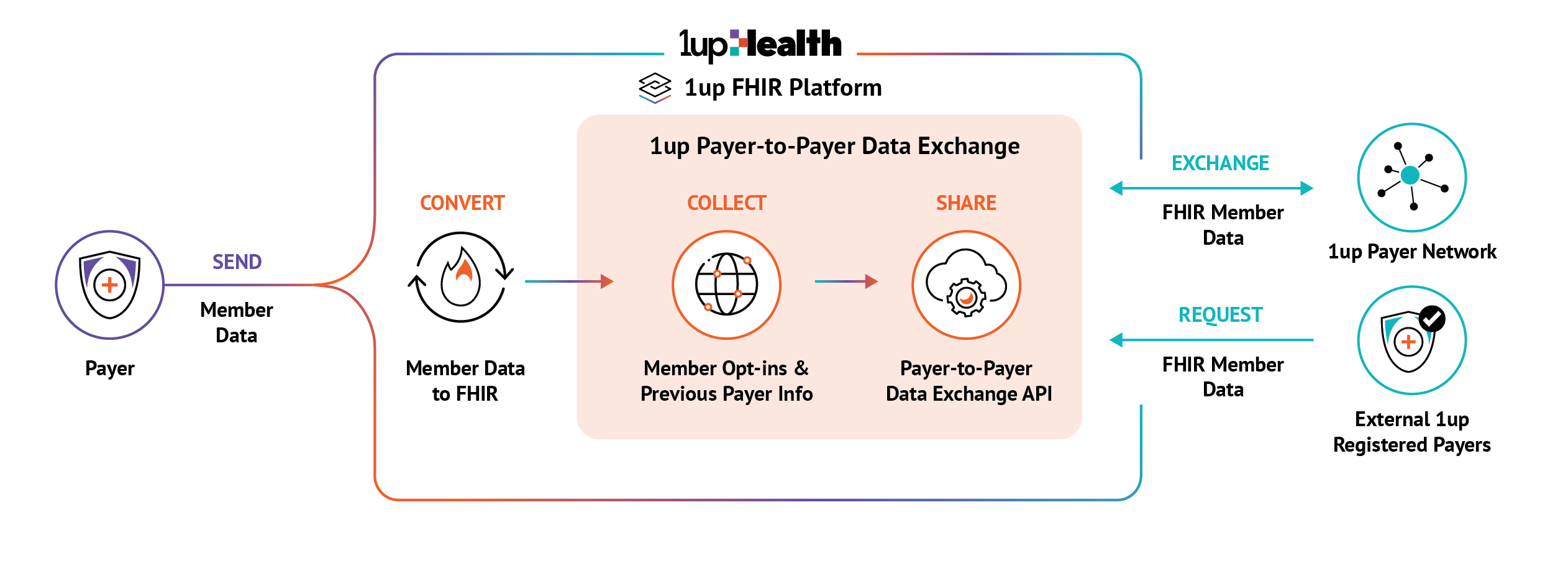
How 1up Payer-to-Payer Data Exchange Works
- Send your member data to the 1up FHIR Platform. It will be converted to FHIR format and exposed via the Payer-to-Payer Data Exchange API.
- Provide 1up with your members’ previous payer information and data-sharing opt-ins.
- Request your members’ historical data from their previous plans through the 1upHealth payer network. When a member’s historical data is received, it is securely integrated with their exist- ing member data for a comprehensive view.
- Scheduled quarterly updates to ensure data for opted-in members with concurrent coverage is kept up to date.
- Payers not on the 1up FHIR Platform can register with 1up and receive scoped access to retrieve member data.
Why 1up Payer-to-Payer Data Exchange
Secure
Accessible only to qualified payers with valid credentials and proper scope of permissions
Standardized
Adheres to the FHIR R4 standard for bulk export and individual FHIR resource APIs
Expansive
Accelerates data exchange with participating payers in 1up’s expansive network
Comprehensive
Combines internal and external member data for a more holistic member view