1UP PLATFORM
The most advanced, FHIR-native health data management platform
The 1up Platform empowers payers to harness the full potential of computable interoperability, transforming how they acquire, manage, and use healthcare data to improve member outcomes, streamline operations, and achieve regulatory compliance.

Unlock the power of computable interoperability to drive measurable business outcomes across your organization.
Computable interoperability turns health data into a continuous, actionable stream, enabling real-time integration and use across systems. Unlike traditional batch-based approaches that rely on static data transfers, this modern method processes data instantly from diverse sources, such as clinical and claims records, and leverages FHIR-standardized, API-powered data formats to ensure seamless and scalable exchange.
By eliminating silos and ensuring continuous access to clean, high-quality data, 1up enables payers to reduce costs, optimize quality and risk programs, improve provider relationships, and support data-driven member experiences.
Make interoperability your competitive advantage.
Transform your data strategy with a platform that turns interoperability into a powerful engine for real-time insights and seamless health data exchange.
Ensure Regulatory Compliance
Stay ahead of evolving regulations, including CMS-0057-F and CMS-9115-F, with our integrated, future-proof interoperability solution.
Eliminate Data Silos
Aggregate clinical and claims data from diverse sources for a unified, real-time view.
Enable Seamless Data Exchange
Securely exchange data using FHIR-standardized, API-driven technology across the entire healthcare ecosystem.
Unlock Powerful Health Analytics
Unlock access to rich, comprehensive data, empowering your advanced analytics and AI/ML tools to deliver deeper insights, reduce risk, enhance quality measures, and drive better patient outcomes.
Deliver Better Patient Outcomes
Improve member care with data-driven decision-making that leads to healthier outcomes.
How the 1up Platform Works
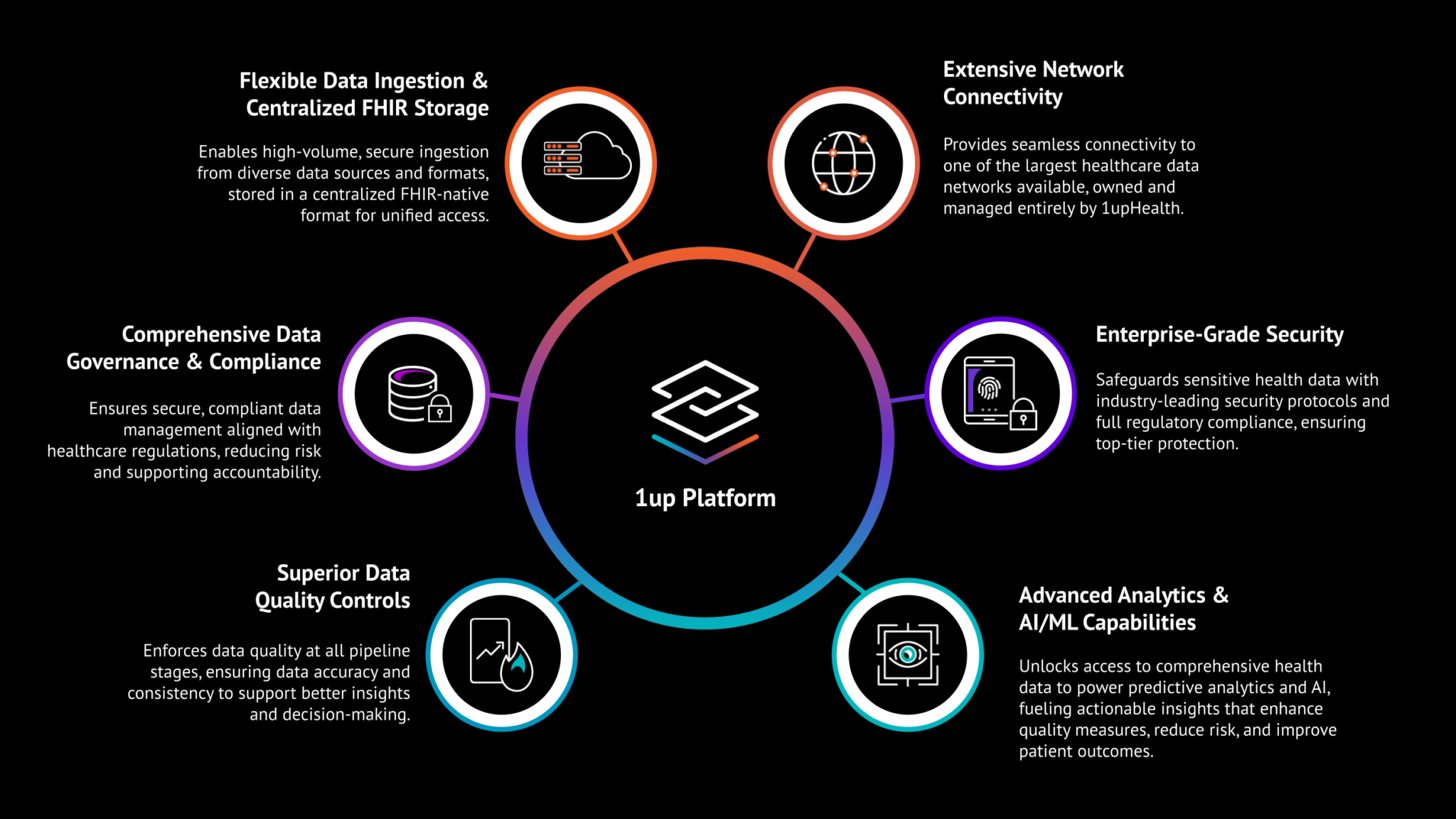
Our cloud-based, API-powered, FHIR®-native platform is designed to enable seamless data exchange across the healthcare ecosystem. It’s purpose-built for healthcare and leverages a modern data lakehouse architecture and big data design patterns to deliver unrivaled data processing efficiency, storage scalability, ingestion flexibility, and data quality.
Backed by 1upHealth’s extensive network of 7,500+ FHIR endpoints, the 1up Platform enables seamless acquisition, management, and exchange of data across payer ecosystems—powering analytics, compliance, and member experience initiatives with ease.
Data Lakehouse Architecture
Purpose Built for Payers
Big Data Scalability & Performance
Future Proof Flexibility
Superior Data Quality
Enterprise Grade Security
Explore Our Products
1up Patient Access
Empower members with easy, secure access to their health data via third-party apps.
1up Provider Access
Seamlessly share member data with your provider partners, boosting satisfaction.
1up Electronic Prior Authorization
Automate end-to-end prior authorization workflows to reduce administrative burden.
1up Payer-to-Payer Data Exchange
Bi-directionally exchange member data with other payers to improve care continuity.